The field of gynecology has transformed dramatically over the last few decades. From traditional open surgeries to advanced minimally invasive and robotic techniques, modern gynecological care is now safer, faster, and more effective than ever before. These innovations not only improve recovery time but also reduce pain, scarring, and hospital stays.
In this article, we’ll explore the most groundbreaking advances in gynecology — focusing on how laparoscopy, robotics, and digital technologies are reshaping women’s health care.
1. The Evolution of Gynecological Surgery
From Open Surgery to Minimally Invasive Techniques
In the past, most gynecological conditions — such as fibroids, cysts, or endometriosis — were treated using open abdominal surgery. These procedures involved large incisions, long recovery periods, and higher risks of complications.
However, with the advent of laparoscopy and robot-assisted surgery, the approach to women’s reproductive surgery has changed drastically. Modern tools allow surgeons to perform complex procedures through tiny incisions, leading to faster recovery and minimal scarring.
2. Laparoscopy: The Foundation of Modern Gynecology
What Is Laparoscopy?
Laparoscopy, often called “keyhole surgery,” uses a thin tube with a camera (laparoscope) inserted through small incisions in the abdomen. It provides a clear, magnified view of the pelvic organs, enabling surgeons to diagnose and treat various gynecological issues with precision.
Common Gynecological Uses
- Ovarian cyst removal
- Treatment of endometriosis
- Hysterectomy (uterus removal)
- Tubal ligation (sterilization)
- Myomectomy (fibroid removal)
Advantages of Laparoscopy
- Smaller incisions and less visible scarring
- Shorter hospital stays
- Quicker recovery
- Reduced post-surgical pain
- Lower infection risk
Laparoscopy revolutionized gynecology and laid the groundwork for even more advanced techniques like robotic-assisted surgery.
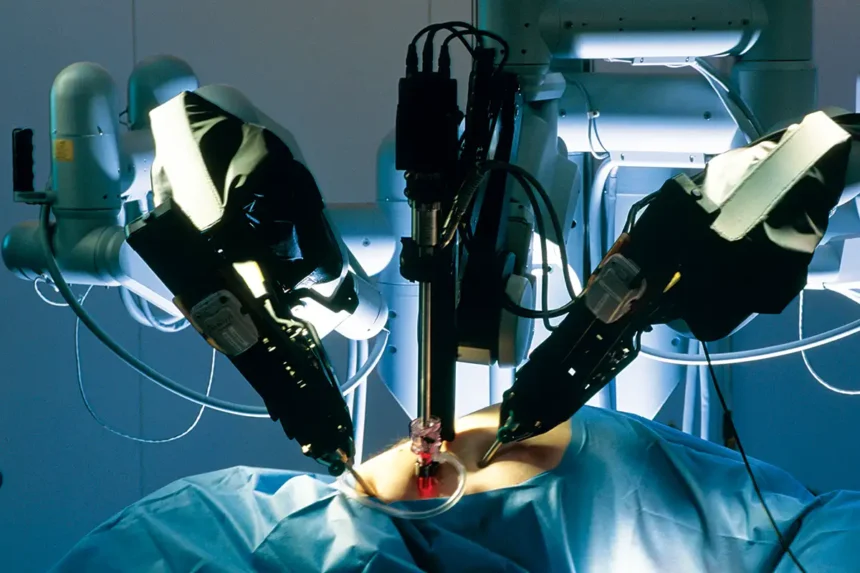
3. Robotic Surgery: The Future of Gynecological Procedures
Understanding Robotic-Assisted Surgery
Robotic surgery represents the next step in gynecological innovation. It combines the skill of experienced surgeons with the precision of advanced robotic systems. One of the most well-known systems is the da Vinci Surgical System, which allows for extreme accuracy and control during surgery.
How It Works
- The surgeon sits at a console and operates robotic arms equipped with surgical tools.
- The system translates the surgeon’s hand movements into micro-motions with unmatched precision.
- A 3D high-definition camera gives an enhanced view of the internal organs.
Procedures Commonly Performed with Robotics
- Hysterectomy
- Myomectomy
- Endometriosis excision
- Pelvic organ prolapse repair
Benefits of Robotic Surgery
- Enhanced precision and dexterity
- Minimal blood loss
- Less post-operative pain
- Faster healing and return to daily activities
- Shorter hospital stays
Robotic surgery is especially beneficial for women with complex conditions or those requiring delicate reconstructive procedures.
4. Hysteroscopy: A Gentle Approach to Uterine Health
Overview
Hysteroscopy involves inserting a small camera (hysteroscope) through the vagina and cervix to examine the inside of the uterus. It’s a minimally invasive technique used for both diagnosis and treatment.
Common Uses
- Investigating abnormal bleeding
- Removing uterine polyps or fibroids
- Diagnosing infertility causes
- Treating intrauterine adhesions
Benefits
- No external incisions
- Same-day procedure in many cases
- Quick recovery and minimal discomfort
Hysteroscopy has become a vital tool in modern gynecology, allowing physicians to treat many uterine conditions without surgery.
5. Advances in Diagnostic Imaging and Screening
High-Resolution Ultrasound and MRI
Today’s imaging technologies have made early diagnosis of gynecological disorders more accurate. High-definition ultrasound, 3D imaging, and MRI scans provide detailed visuals of pelvic organs, helping detect conditions like fibroids, cysts, and cancers early on.
Molecular and Genetic Testing
Genetic and molecular testing now plays a key role in detecting inherited gynecological cancers, such as ovarian and endometrial cancer. This allows women with a family history of such diseases to take preventive action sooner.
HPV Testing and Cervical Screening
Modern gynecology emphasizes HPV DNA testing alongside Pap smears to improve early detection of cervical cancer. These screening tools have dramatically reduced cervical cancer rates worldwide.
6. Fertility-Preserving and Reproductive Technologies
Assisted Reproductive Technologies (ART)
Technological breakthroughs have also advanced fertility treatments. Procedures such as In Vitro Fertilization (IVF), Intrauterine Insemination (IUI), and Egg Freezing are now more successful and accessible.
Laparoscopic Fertility Surgery
Minimally invasive laparoscopic techniques are used to treat blocked fallopian tubes, endometriosis, and ovarian cysts — all while preserving fertility.
Uterus Transplant and Stem Cell Research
Recent research in uterine transplantation and stem cell therapy is paving the way for new fertility restoration options for women who were previously unable to conceive.
7. Digital and AI Integration in Gynecology
Artificial Intelligence (AI) in Diagnosis
AI-powered algorithms are now used to analyze ultrasound and imaging data, improving diagnostic accuracy for conditions like ovarian cancer and PCOS.
Tele-Gynecology
The rise of telemedicine has made it easier for women to consult gynecologists remotely, especially in underserved areas. Digital platforms allow virtual consultations, follow-up visits, and online monitoring of reproductive health.
Wearable Health Devices
Smart wearable devices now track menstrual cycles, fertility windows, and hormonal changes — empowering women to manage their reproductive health proactively.
8. Enhanced Pain Management and Recovery Techniques
Minimally Invasive Anesthesia Methods
Advancements in anesthesia have made gynecological surgeries safer and more comfortable, with fewer side effects.
Fast-Track Recovery Programs
Enhanced Recovery After Surgery (ERAS) programs help patients resume normal activities quickly by reducing hospital stays, optimizing nutrition, and controlling post-operative pain effectively.
Conclusion
Modern gynecology has entered an era defined by innovation, precision, and patient-centered care. From laparoscopy to robotic surgery, these advances have transformed the way gynecological diseases are diagnosed and treated. Women now benefit from safer procedures, quicker recovery, and improved outcomes.
As technology continues to evolve — with AI, genetics, and robotics leading the way — the future of gynecology promises even greater advancements, empowering women with better health, confidence, and quality of life.